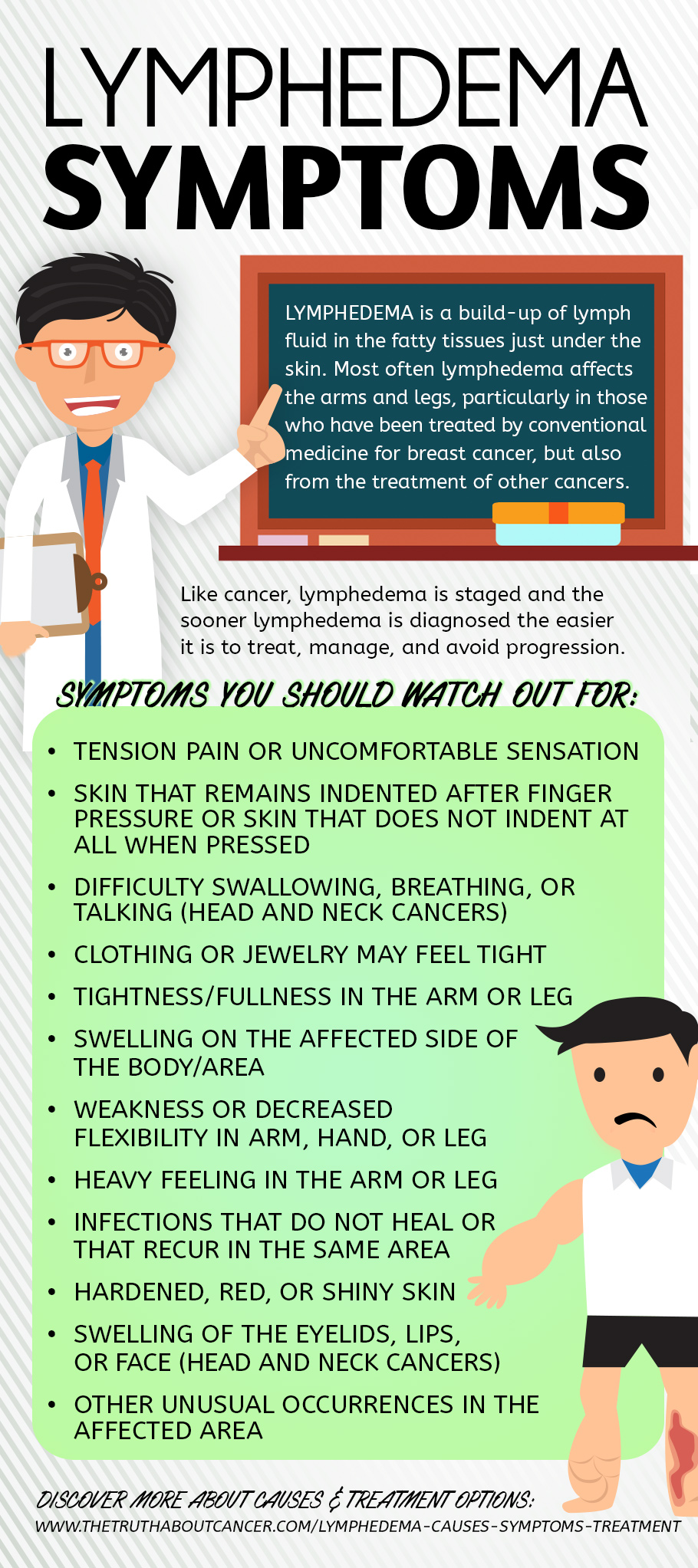
Lymphedema is a build-up of lymph fluid in the fatty tissues just under the skin. Most often lymphedema affects the arms and legs, particularly in those who have been treated by conventional medicine for breast cancer, but also from the treatment of cancers of the bladder, kidneys, and other lower extremity cancers.
In this article we’ll examine lymphedema causes, symptoms of lymphedema, and lymphedema treatment options that are available to those suffering from the condition.
Lymphedema Causes
Lymphedema is a common complication of certain conventional cancer treatments which your doctor may not have warned you about.
Cancer tests & treatments that could possibly lead to lymphedema are:
- Mastectomy
- Lumpectomy
- Lymph node removal or biopsy
- Radiation treatment
- Use of the drug Tamoxifen
While the medical community dismisses lymphedema as “an unfortunate side effect,” the resulting condition impairs quality of life and increases the risk of serious infections such as cellulitis and erysipelas.
Many people are not aware that lymphedema can occur at any time, even 30 years later, although typically it occurs between one to three years after surgery and/or radiation. Infections, chemotherapy, and drugs such as Tamoxifen have also been implicated in the development of lymphedema. Biopsies raise the risk of lymphedema as they damage nodes and lymphatic pathways and increase the risk of infection.
Who’s at Risk for Developing Lymphedema?
- Women and men who have breast cancer and have lymph nodes removed and/or who have had radiation therapy are at risk of getting lymphedema. The condition affects about one in five women (20%) who have breast surgery and/or radiation therapy. There’s an even higher risk for those who have had both lymph node removal surgery and radiation treatment.
- Lymphedema can also occur in women with ovarian and/or cervical cancer if treated with radiation therapy which impairs inguinal nodes (those in the groin).
- Lymphedema can also be a complication of conventional treatment for head and neck cancer, creating problems such as difficulty swallowing, vocal cord swelling, and swelling of the face, jaw, and neck.
Common Lymphedema Symptoms
As pertains to all cancers, lymph swelling is usually gradual and may occur in just one part of the leg, arm or hand, or throughout. The swelling can range from mild to severe. Risk of lymphedema is typically limited to the side or area of the body where cancer is present and/or was treated.
Possible Symptoms of Lymphedema include:
- Swelling on the affected side of the body/area
- Clothing or jewelry may feel tight
- Tightness/fullness in the arm or leg
- Weakness or decreased flexibility in arm, hand, or leg
- Tension pain or uncomfortable sensation
- Skin that remains indented after finger pressure OR skin that does not indent at all when pressed
- Hardened, red, or shiny skin
- Heavy feeling in the arm or leg
- Infections that do not heal or that recur in the same area
- Swelling of the eyelids, lips, or face (head and neck cancers)
- Difficulty swallowing, breathing, or talking (head and neck cancers)
- Other unusual occurrences in the affected area
Like cancer, lymphedema is staged and the sooner lymphedema is diagnosed the easier it is to treat, manage, and avoid progression. Late stage lymphedema can lead to fibrosis, which presents as hard and dense skin. Fibrosis can eventually lead to vascular problems and increased risk of serious infection.
6 Foundational Lymphedema Treatments
There is no pill that will prevent or correct lymphedema, but there are steps you can take to reduce your risk of lymphedema and to manage the condition.
The following are some ways for preventing flare ups, managing symptoms, and reducing your risk of developing lymphedema:
- Manual Lymphatic Drainage (MLD) – a type of gentle skin massage that helps move lymphatic fluids. This is done by a lymphedema specialist and is typically covered by insurance.
- Complete Decongestive Therapy (CDT) – often considered the main treatment for lymphedema by the medical community, CDT is a multi-phase treatment that includes MLD, exercise, compression, and skin care, and should be performed by a therapist who specializes in lymphedema.
- Acupuncture – studies have shown acupuncture relieves pain and swelling from lymphedema. EFT (Emotional Freedom Technique) and other energy approaches may help as well.
- Self-massage – There are ways to massage, or “milk” the lymphatics. Seek guidance from a qualified lymph specialist. There are also many resources available online.
- Low Level Laser Therapy (LLLT) – increases the movement of lymph, breaks down scar tissue, and brings relief from symptoms. Laser therapy was approved by the U.S. Food and Drug Administration in 2006 for the treatment and management of lymphedema, but is still considered controversial by many as studies have been inconclusive. This treatment is best done by a health professional who specializes in lymphedema. Medical insurance typically pays for part of the cost of treatment.
- Hydrotherapy – the therapeutic use of water helps improve circulation and may reduce lymphedema symptoms. Exercise in a comfortable water temperature (not hot) for approximately 20 to 60 minutes. A hydrotherapy session with a lymphedema physiotherapist may be helpful for developing an exercise plan.
- Essential oils – concentrated oils from plants such as frankincense, myrrh, and ginger promote lymphatic movement. Essential oil of lemon, frankincense, and lavender help to dissolve petrochemicals and remove heavy metals so the body can eliminate them. Apply oils to the affected area twice a day, as well as to the bottom of the feet before bed. (Be careful as oils can be slippery, so do this bedside and right before retiring.) Only use the highest quality organic oils from a trusted source.
- Horse Chestnut – this herb may be useful with lymphedema, along with other herbs such as burdock root, red clover, and echinacea with or without goldenseal.
- Selenium has been helpful for those with head and neck cancers.
- Oregano oil supports the immune system and is helpful for digestive support. The terpenes in oregano oil help dissolve fatty sludge in the lymph system.
- Bromelain – a proteolytic (protein-digesting) enzyme found in pineapple stems that has anti-inflammatory, anticoagulant, and diuretic effects.
- Adding enzyme rich foods to meals such as pineapple, papaya, kiwi, avocado, raw honey, bee pollen, extra virgin olive oil, and coconut oil is healthy and can be helpful.
- Proteolytic enzymes – These facilitate the chemical breakdown of proteins and process material in the circulatory and lymph systems, essentially cleaning out the blood.
- Castor oil – helps to improve the lymphatic flow; it increases circulation of lymphatic fluids, reduces inflammation and improves digestion. Apply the oil to different parts of the skin; especially to the lower abdomen. Castor oil is a thick oil, and is best to apply before bed. Place a towel over your sheets or wear old pajamas.
- Cabbage leaf packs – Using cabbage leaf compresses for breast engorgement after childbirth dates back hundreds of years. Many have found this old, natural remedy brings relief from lymphedema swelling as well. Be sure to use clean, organic cabbage leaves and don’t use on broken or irritated skin.
- Detoxification and liver support – Efficient liver function is essential to the lymphatic system.
- Visualization – a form of meditation, visualization has been helpful for many. Sit comfortably, breath and visualize excess fluids draining from the body. This should only take five minutes.
Should You Wear Compression Garments With Lymphedema?
There are a variety of compression garments on the market including gloves, stockings, vests, and shorts. While long recommended, this is still an open question as to whether or not these really help.
One time when compression garments may be particularly helpful, however, is during air travel. The decreased cabin pressure may increase swelling as diminished cabin pressure will hinder fluid movement in the lymphatic system. While compression garments are still controversial, many people do find wearing one during travel is beneficial.
Last Resort If Other Lymphedema Interventions Don’t Bring Relief
- Microsurgery – for transplanting lymph nodes, vessels, and the creation of artificial lymph nodes is being examined. Case studies have shown that for those with a lack of response from more conservative treatments, surgical therapies offer promising results.
- Lymph node transplants
- Compression pumps
- Hyperbaric oxygen therapy (HBOT) – studies have shown HBOT to be effective for some people with lymphedema as it supports lymphangiogenesis, the formation of lymphatic vessels from preexisting lymphatic vessels. HBOT requires access to specialized hyperbaric chambers and the ability to handle time spent in a pressurized chamber.
Lifestyle Modifications to Lower Lymphedema Risk
In addition to lifestyle practices that support good lymphatic function, it is also advisable to take some simple precautions to minimize risk of injury, infection, or anything that promotes the development of lymphedema.
Ways to minimize lymphedema risks during activities:
- Gardening – use gardening gloves to avoid injuring the skin.
- Sunbathing – avoid sunburn as it places an extra burden on the lymphatic system. Use non-toxic sunscreens when out in the sun.
- Manicures – bring your own tools, don’t cut your cuticles, and keep skin well moisturized. Bacteria and fungus can enter the skin via cracks and dry areas, which can result in infection. Skin infections such as cellulitis, for example, can be serious for those with lymphedema.
- Jacuzzis – dangle only your feet; hot water causes vasodilation, which is the expansion of blood vessels. This expansion increases the flow of fluid from blood vessels into tissue, increasing swelling. Hot tubs harbor bacteria, so avoid completely if you have even a small cut or cracked skin (also see note below about avoiding raising your core body temperature).
- Avoid saunas and hot baths – both raise your core body temperature which can increase swelling, and can actually cause the development of lymphedema. Warm baths are considered fine, but limit to 15 minutes and keep the water temperature below 102 degrees Fahrenheit.
- Do your best to avoid mosquito and other insect bites – use non-toxic insect repellents, wear protective covering, and/or avoid being outside at dawn and after dusk.
- Remind medical professionals to draw blood and place pressure cuffs only on the unaffected arm or least affected arm or use the thigh.
Lymphedema is not just a pesky side effect. It can be a serious condition that can have life-long consequences – significantly reducing your quality of life and, in some cases, increasing mortality. Use this information to reduce your personal risk, and if you already have lymphedema, incorporate best practices to manage it before it progresses.
Want to stay abreast of new ways to stay healthy? Be notified each week when cutting-edge articles are added by clicking here. You’ll be glad you did.
Article Summary
Lymphedema is a build-up of lymph fluid in the fatty tissues just under the skin.
Cancer tests & treatments that could possibly lead to lymphedema are:
- Mastectomy
- Lumpectomy
- Lymph node removal or biopsy
- Radiation treatment
- Use of the drug Tamoxifen
Those at risk of developing lymphedema include:
- Those who have lymph nodes removed and/or receive radiation therapy
- Women who receive radiation therapy for ovarian or cervical cancer
- Anyone receiving conventional treatment for head and neck cancer
Possible symptoms of lymphedema include:
- Swelling on the affected side of the body/area
- Clothing or jewelry may feel tight
- Tightness/fullness in the arm or leg
- Weakness or decreased flexibility in arm, hand, or leg
- Tension pain or uncomfortable sensation
- Skin that remains indented after finger pressure or skin that does not indent at all when pressed
- Hardened, red, or shiny skin
- Heavy feeling in the arm or leg
- Infections that do not heal or that recur in the same area
- Swelling of the eyelids, lips, or face (head and neck cancers)
- Difficulty swallowing, breathing, or talking (head and neck cancers)
- Other unusual occurrences in the affected area
6 foundational lymphedema treatments:
- Manual Lymphatic Drainage (MLD)
- Complete Decongestive Therapy (CDT)
- Acupuncture
- Self-massage
- Low Level Laser Therapy (LLLT)
- Hydrotherapy
Last resort treatments include:
- Microsurgery
- Lymph node transplants
- Compression pumps
- Hyperbaric oxygen therapy (HBOT)
Ways to minimize lymphedema risks:
- Wear gloves when gardening
- Avoid sunburn and use non-toxic sunscreen
- If receiving manicures bring your own tools, don’t cut your cuticles, and keep skin well moisturized
- Avoid Jacuzzis, saunas, and hot baths
- Avoid insect bites
- Remind medical professionals to draw blood and place pressure cuffs only on the unaffected arm





















Hello Family; Thank you Ty for bring this to our awareness. Another tool that may help the Lymph’s is a up and down movement as a re bounder and skipping with or without a rope if you can or a more gentle up and down like dancing or moving to music. And using visualization to imagine yourself doing these things, but make it as real as you can,and there maybe a emotional cause to all of this. Just sharing and Loving. alan.
We cansurvivors often have to handle lymphodema and there are other strategies on the cansurviving site including Epsom salts baths! Heaven with some frankincense oil in the warm water and then just soak…try visiting the site?
Maybe practicing Yoga might help with the lymph nodes. Dancing around it circles might help because one is moving his or her’s arms or legs.
Does Epigenetic labs plan on eventually adding myrrh essential oil? If not what is a good company that produces pure and non-toxic healthy myrrh oil?
Thank you for this! My stage 1, NO lymph node involvement breast cancer op Sept 2012 resulted in FORCED radiation (I told the therapist half way through the 5 week daily radiation that I had changed my mind and DID not want any more I wept and “they” called their head who “forced” me to continue.) I didn’t have the strength to resist. I had already refused to continue with the Tamoxafin after the first bottle and 3 pills! Going to my last recent check up in January 2017, the Prof told me I had lymphodema and sent me to a physio. Thank the Lord it is NOT bad and so grateful for this article. Thank you Ty. God bless you and your organization. Grateful Glenda in Port Alfred, South Africa
Some good information. Compression bandaging and well fitting compression garments are a vital part of CDT Treatment/ long term management and reducing the progression of the condition. The jury is not out on this. The other things mentioned like oils and diet and possibly others are worth adding to the management plan.
I found with one patient who had a sightly sore and stiff arm after breast cancer seven years previously that ear candling helped greatly. This sounds odd but if you understand that candling stimulates the lymph system it is easy to see how it could help the lymph to drain correctly. And it is a treatment that couldn’t be more gentle.
Sometimes I scratch my head in my sleep. Weird, right? I also sleepwalk. Anyway, I had an itchy head and scratched it raw. The lymphnodes on my upper neck got infected, cellulitis. Dr. put me on antibiotics. A few days later my arms and legs got all swollen and hard, especially if I left them down. Freaked me out when I realized there was fluid moving under my skin. A week or so later it went away. Should I be worried about cancer?
LET therapy (lymphatic enhancement therapy is another helpful way to help open the lymph system. Relaxing and effective. In the DFW area call Nancy at(972) 978-6803 .
I have Lymphedema and find the medical field (insurances) don’t recognize it. I do my own exercises and I wear a compression sleeve and gauntlet all waking hrs and a night sleeve when in bed. I also received a pump from a therapist I was lucky enough to find for an emergency massage. I have had this for 6 yrs now and I sure wish someone would come up with a cure. It is very debilitating.
Does Megace cause lymphedema? I developed it in one leg after taking it for about a month or 2. According to this article possibly tamoxifin can cause lymph edema. I would be so grateful for an answer.
Cathy